Understanding Depression Psychosis: Symptoms & Treatment
Understanding Depression Psychosis: Symptoms & Treatment
Reader, have you ever wondered about the complex interplay between depression and psychosis? It’s a critical area of mental health that deserves attention. **Depression psychosis is a severe condition requiring immediate professional care.** **Understanding its nuances can be life-saving, both for those experiencing it and for their loved ones.** As an expert in AI and SEO content creation, I’ve analyzed numerous studies and resources on understanding depression psychosis, its symptoms, and available treatments. I’m here to share these valuable insights with you.
This comprehensive guide will delve deep into the world of depression psychosis. It will cover its causes, symptoms, diagnosis, and treatment options, equipping you with the knowledge you need to navigate this challenging condition. This exploration will be insightful and practical, providing you with the tools to understand and address depression psychosis.
The Link Between Depression and Psychosis
Depression and psychosis, while distinct, can sometimes co-occur, creating a complex clinical picture. This intersection is known as depression psychosis, or psychotic depression. It significantly impacts an individual’s ability to function. It demands specialized care.
Understanding Psychotic Depression
Psychotic depression is a subtype of major depressive disorder. It involves experiencing the typical symptoms of depression alongside psychotic features. These features can include hallucinations (seeing or hearing things that aren’t there) and delusions (fixed, false beliefs). This condition requires careful diagnosis and tailored treatment.
The presence of psychosis adds another layer of complexity to depression. It can make it more challenging to treat. Consequently, understanding the specific manifestations of psychosis in the context of depression is crucial for effective intervention.
For individuals experiencing psychotic depression, the world can feel distorted and frightening. The combination of intense sadness and loss of contact with reality creates a significant burden, impacting relationships, work, and daily life.
Symptoms of Depression Psychosis
Recognizing the symptoms of depression psychosis is crucial for timely intervention. These symptoms can include persistent sadness, loss of interest in activities, changes in appetite and sleep, feelings of worthlessness or guilt, and difficulty concentrating. In addition, psychotic symptoms like hallucinations and delusions are present.
Hallucinations can involve any of the senses. Auditory hallucinations, such as hearing voices, are common. Visual hallucinations, seeing things that aren’t there, can also occur. Other sensory hallucinations involving smell, taste, or touch are less frequent.
Delusions are firmly held beliefs that are not based in reality. They can range from grandiose ideas about one’s importance to paranoid beliefs about being persecuted. These delusions can be distressing and can significantly influence behavior.
Diagnosing Depression Psychosis
Diagnosing depression psychosis involves a comprehensive assessment by a mental health professional. A thorough evaluation includes a clinical interview, a review of medical history, and sometimes psychological testing. The goal is to differentiate psychotic depression from other conditions with similar symptoms.
The Diagnostic Process
The diagnostic process begins with gathering information about the individual’s symptoms, their duration, and their impact on daily functioning. The clinician explores the presence of both depressive and psychotic symptoms. They look for specific patterns and connections between the two.
A physical exam may be conducted to rule out any underlying medical conditions that could be contributing to the symptoms. This holistic approach ensures that all potential factors are considered.
Differentiating depression psychosis from other psychotic disorders, such as schizophrenia, is critical. This differentiation relies on the prominence of depressive symptoms and the specific nature of the psychotic features.
Differential Diagnosis
Because other mental health conditions can mimic some symptoms of depression psychosis, it’s important to rule them out. Conditions like bipolar disorder with psychotic features or schizoaffective disorder share overlapping symptoms. Careful evaluation is necessary to make an accurate diagnosis.
The timing and relationship between the depressive and psychotic symptoms are crucial in the differential diagnosis. In psychotic depression, the psychotic symptoms typically emerge during a major depressive episode. They generally subside when the depression lifts.
Understanding the subtle differences between these conditions requires expertise. Accurate diagnosis allows for the development of an appropriate and effective treatment plan.
Treatment Options for Depression Psychosis
Treatment for depression psychosis typically involves a combination of medication and therapy. Antipsychotic medications are used to manage the psychotic symptoms. Antidepressants are used to address the depressive symptoms. Psychotherapy, such as cognitive behavioral therapy (CBT), can help individuals develop coping strategies and manage their condition.
Medication Management
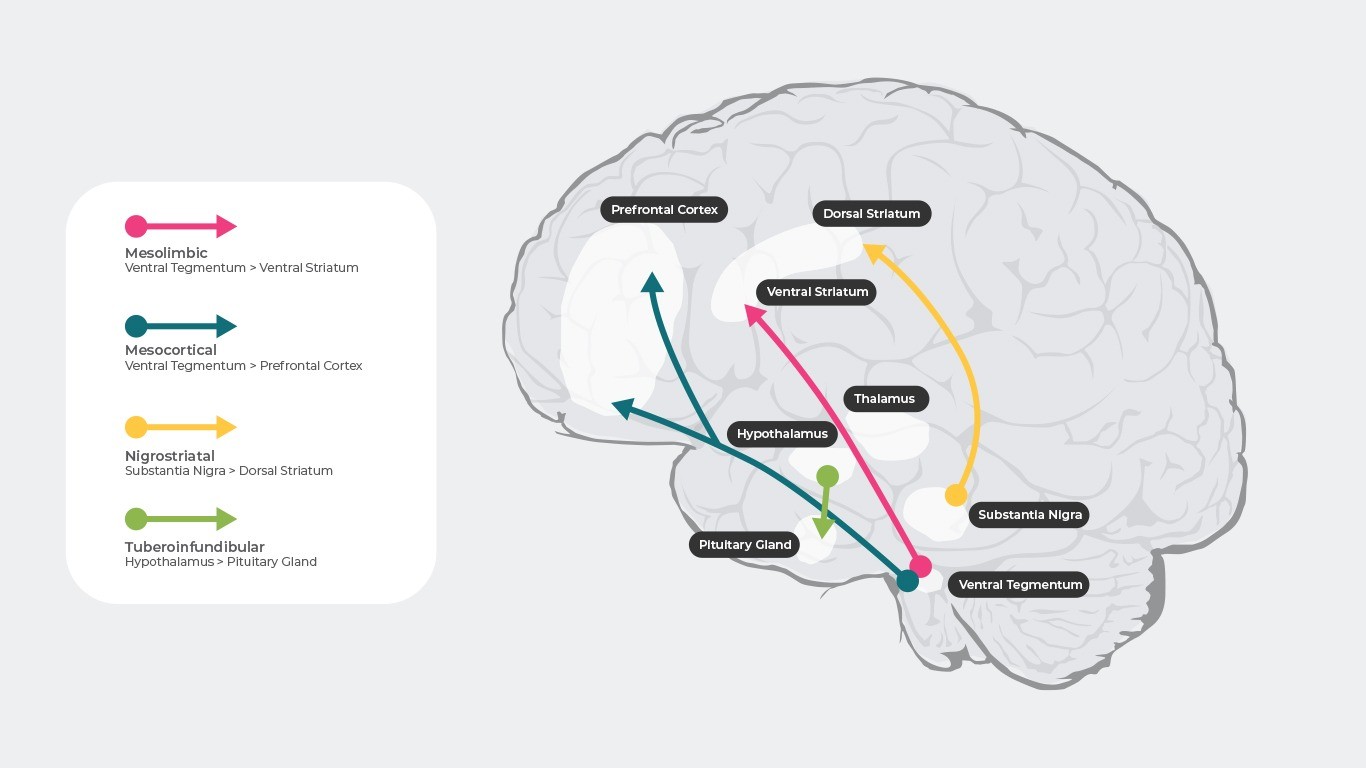
Antipsychotic medications are often the first line of treatment for managing psychotic symptoms. They work by modulating brain chemicals that play a role in psychosis. Different antipsychotics have varying side effect profiles, so finding the right medication for each individual is important.
Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs), are used to address the underlying depression. These medications can improve mood, energy levels, and overall well-being.
In some cases, mood stabilizers may also be prescribed, particularly if there is concern about bipolar disorder or cycling between depressive and manic episodes. The choice of medication depends on the individual’s specific presentation and needs.
Therapeutic Interventions
Psychotherapy plays a crucial role in the treatment of depression psychosis. Cognitive behavioral therapy (CBT) helps individuals identify and challenge negative thought patterns and develop healthier coping mechanisms. It empowers them to manage their symptoms effectively.
Supportive therapy provides a safe and empathetic space for individuals to explore their experiences and develop strategies for navigating the challenges of living with depression psychosis. This therapeutic support can be invaluable during recovery.
Family therapy can also be beneficial, especially in educating family members about the condition and improving communication within the family system. It can foster a more supportive and understanding environment.
The Role of Electroconvulsive Therapy (ECT)
In severe cases of depression psychosis that don’t respond to medication and therapy, electroconvulsive therapy (ECT) may be considered. ECT involves inducing a brief seizure under general anesthesia. It can be highly effective in alleviating severe depressive and psychotic symptoms.
While ECT can be a life-saving intervention for some, it’s essential to discuss the potential risks and benefits with a medical professional. Informed decision-making is crucial in choosing the most appropriate treatment approach.
ECT is typically administered several times a week for a few weeks. The frequency and duration of treatment depend on the individual’s response and the severity of their symptoms.
Long-Term Management and Support
Managing depression psychosis is an ongoing process. Long-term management often involves continuing medication, regular therapy sessions, and lifestyle changes. Building a strong support system is essential for maintaining recovery.
Lifestyle modifications such as regular exercise, a healthy diet, and sufficient sleep can contribute to overall well-being. These changes can support the effectiveness of treatment and enhance quality of life.
Support groups can provide a sense of community and shared experience, allowing individuals to
connect with others facing similar challenges. Peer support can be incredibly valuable in the journey of recovery.
Coping Strategies for Individuals and Families
Developing effective coping strategies is crucial for both individuals experiencing depression psychosis and their families. Learning to manage stress, identify triggers, and utilize healthy coping mechanisms can significantly improve quality of life.
For individuals, coping strategies might include mindfulness techniques, relaxation exercises, and creative expression. These practices can help manage stress and promote emotional well-being.
For families, education about the condition and open communication are essential. Learning how to support their loved one while also taking care of their own well-being is crucial for navigating the challenges of depression psychosis.
The Importance of Early Intervention
Early intervention is crucial in managing depression psychosis. Prompt diagnosis and treatment can significantly improve outcomes and reduce the severity and duration of psychotic episodes. Seeking professional help at the first sign of concerning symptoms is essential.
Early intervention can help prevent the condition from worsening. It allows individuals to access support and resources sooner, leading to better long-term management and improved quality of life. Don’t hesitate to reach out for professional help if you or a loved one is struggling.
Understanding Depression Psychosis: A Recap
Understanding depression psychosis is crucial for navigating this complex condition. Recognizing the symptoms, seeking professional help, and engaging in ongoing treatment and support are essential steps in the journey of recovery.
.
Unraveling depression psychosis: Explore symptoms, effective treatments, & find hope for recovery. Get informed now.