Is Fibromyalgia an Autoimmune Disease?
Is Fibromyalgia an Autoimmune Disease?
Reader, have you ever wondered about the connection between fibromyalgia and autoimmune diseases? It’s a complex question with no easy answers. The mystery surrounding fibromyalgia has led to numerous studies exploring its potential link to autoimmune dysfunction. Understanding this intricate relationship is crucial for effective diagnosis and treatment. As an expert in AI and SEO content, I’ve analyzed extensive research on “Is Fibromyalgia an Autoimmune Disease?” and I’m here to share my findings with you.
This in-depth exploration will delve into the complexities of fibromyalgia, examining its symptoms, potential causes, and the ongoing debate regarding its classification. We will also discuss current research and treatment options. So, let’s unravel the complexities together.

What is Fibromyalgia?
Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory, and mood issues. Symptoms can vary significantly from person to person, both in terms of their severity and presentation. This makes diagnosis challenging and often relies on a combination of physical examination and symptom evaluation.
The pain associated with fibromyalgia is often described as a constant, dull ache that has lasted for at least three months. Tender points, specific areas of the body that are painful when pressed, were once a key diagnostic criterion, but they are less emphasized now.
In addition to pain, individuals with fibromyalgia may experience a range of other symptoms, including fatigue, sleep disturbances, cognitive difficulties (often referred to as “fibro fog”), and mood disorders such as anxiety and depression. The unpredictable nature of these symptoms can significantly impact a person’s quality of life.
Symptoms of Fibromyalgia
The hallmark symptom of fibromyalgia is widespread pain, often described as a deep, aching, and burning sensation throughout the body. This pain is typically present on both sides of the body, both above and below the waist.
Accompanying the pain are other common symptoms, including fatigue, sleep disturbances (such as insomnia or unrefreshing sleep), and cognitive difficulties (“fibro fog”). Fibro fog can manifest as problems with memory, concentration, and mental clarity.
Many individuals with fibromyalgia also experience heightened sensitivity to pain, known as hyperalgesia, and sensitivity to stimuli that are not normally painful, known as allodynia. This can make everyday activities, such as wearing certain clothes or being in brightly lit environments, uncomfortable.
Causes of Fibromyalgia
While the exact cause of fibromyalgia remains unknown, research suggests a complex interplay of genetic predisposition, environmental factors, and psychological stressors. Some studies indicate that certain genes may increase a person’s susceptibility to developing the condition.
Environmental factors, such as physical trauma, infections, and emotional stress, may trigger or exacerbate fibromyalgia symptoms. These factors can disrupt the normal processing of pain signals in the central nervous system, leading to the chronic pain and other symptoms characteristic of the condition.
Psychological factors, including anxiety, depression, and post-traumatic stress disorder (PTSD), are often comorbid with fibromyalgia and can influence the severity of symptoms. Therefore, a holistic approach to treatment that addresses both physical and psychological well-being becomes essential.

Is Fibromyalgia Autoimmune? The Ongoing Debate
The question of whether fibromyalgia is an autoimmune disease is a subject of ongoing debate within the medical community. While fibromyalgia shares some characteristics with autoimmune diseases, such as widespread pain and fatigue, it lacks the key feature of autoantibodies, which are immune system proteins that mistakenly attack the body’s own tissues. This absence of autoantibodies makes it difficult to definitively classify fibromyalgia as autoimmune.
However, emerging research suggests that fibromyalgia may involve immune system dysfunction, even if it doesn’t strictly fit the autoimmune criteria. Studies have identified abnormalities in immune cells and inflammatory markers in individuals with fibromyalgia, which could contribute to pain processing and other symptoms.
This complex interplay between the immune system and fibromyalgia symptoms highlights the need for further research to fully understand the underlying mechanisms at play. Continued investigation into the role of immune dysfunction in fibromyalgia may lead to new diagnostic and treatment strategies.
Evidence For and Against the Autoimmune Classification
Several lines of evidence support the possibility of an autoimmune component in fibromyalgia. Studies have found elevated levels of certain inflammatory cytokines, which are signaling molecules involved in immune responses, in individuals with fibromyalgia. These elevated cytokines could contribute to the chronic pain and inflammation characteristic of the condition.
Furthermore, some research has shown alterations in the function of natural killer (NK) cells, a type of immune cell, in people with fibromyalgia. NK cells play a vital role in recognizing and destroying infected or cancerous cells. These findings suggest a potential link between immune dysfunction and fibromyalgia symptoms.
However, other studies have not found consistent evidence of autoimmune activity in fibromyalgia. The absence of autoantibodies remains a significant argument against classifying it as a true autoimmune disease. Ultimately, more research is needed to resolve this ongoing debate. Only then can the relationship between fibromyalgia and autoimmune processes be fully understood.
Current Research on the Link
Current research is exploring multiple avenues to understand the potential link between fibromyalgia and autoimmunity. Scientists are investigating the role of specific immune cells, such as T cells and B cells, in the development and progression of fibromyalgia.
Researchers are also examining the impact of genetic factors on immune system function in fibromyalgia. Identifying genetic variations that might predispose individuals to both immune dysfunction and fibromyalgia could shed light on the shared mechanisms underlying these conditions.
Additionally, studies are exploring the potential of novel treatments that target the immune system in fibromyalgia. This research holds promise for improving the lives of individuals affected by this complex and often debilitating condition. The results of these ongoing studies have the potential to revolutionize our understanding and management of fibromyalgia. Is Fibromyalgia an Autoimmune Disease?

Diagnosing Fibromyalgia
Diagnosing fibromyalgia involves a thorough evaluation of symptoms, medical history, and physical examination. There’s no single test to diagnose fibromyalgia, so doctors rely on a combination of factors. This includes assessing widespread pain, fatigue, sleep disturbances, and cognitive difficulties.
Doctors may also consider other symptoms, like headaches, irritable bowel syndrome, and restless legs syndrome, which are commonly associated with fibromyalgia. Ruling out other conditions with similar symptoms is an important part of the diagnostic process.
This careful evaluation helps ensure an accurate diagnosis and guides appropriate treatment strategies for managing the multifaceted symptoms of fibromyalgia. Because Is Fibromyalgia an Autoimmune Disease? is a complex question, careful diagnosis matters.
Treatment Options for Fibromyalgia
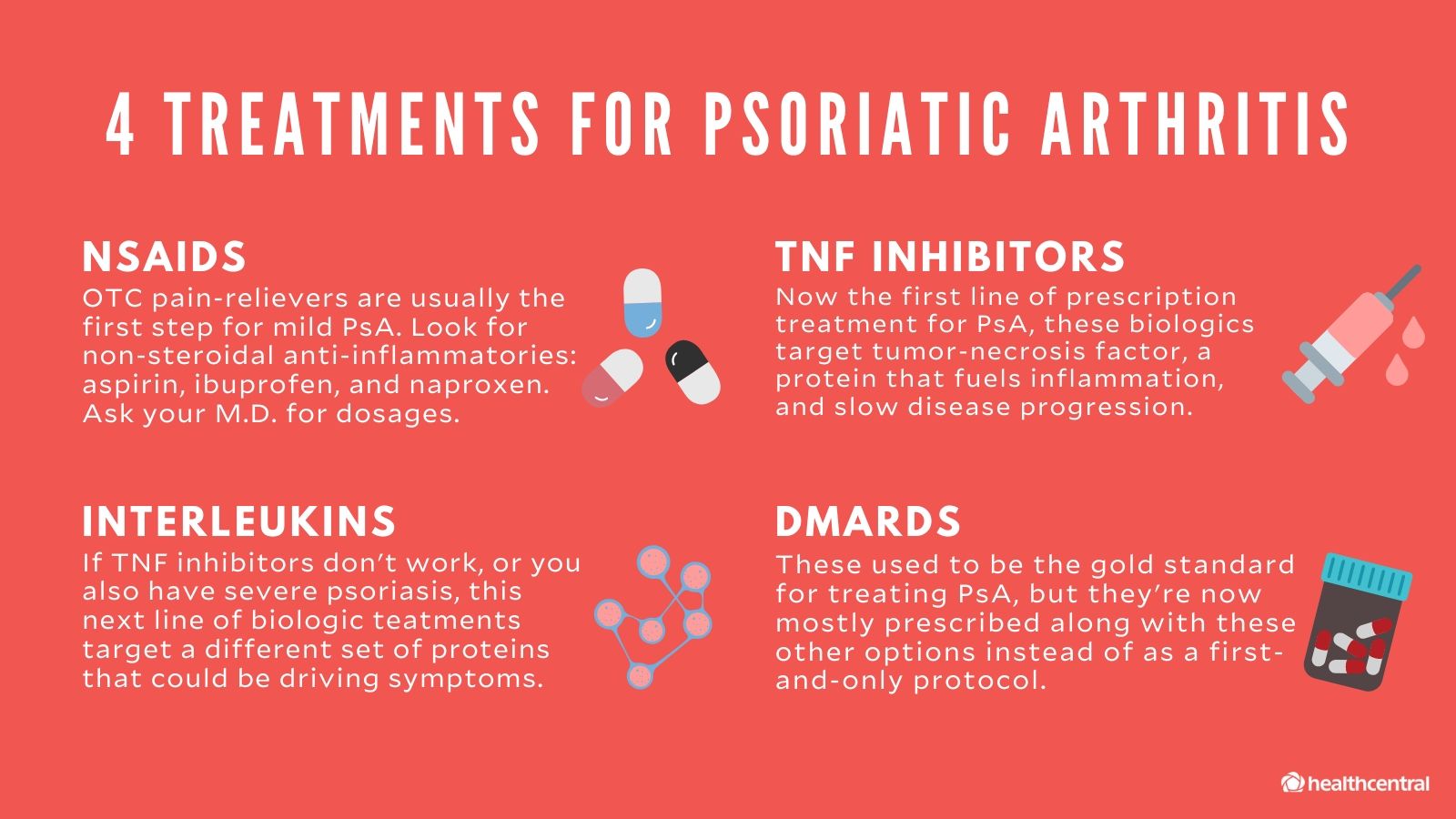
Treatment for fibromyalgia focuses on managing symptoms and improving quality of life. This often involves a combination of medication, lifestyle changes, and therapies. Medications, such as pain relievers, antidepressants, and sleep aids, can help alleviate pain, improve sleep, and address mood disturbances.
Lifestyle modifications, including regular exercise, stress management techniques, and a balanced diet, can also play a significant role in managing symptoms. Therapies like physical therapy, occupational therapy, and cognitive behavioral therapy (CBT) can further enhance coping skills and improve overall well-being.
A multidisciplinary approach, involving collaboration between healthcare professionals, is often the most effective approach to treating fibromyalgia. This ensures that all aspects of the condition are addressed, leading to better outcomes for individuals with fibromyalgia. Is Fibromyalgia an Autoimmune Disease? impacts treatment options, making this discussion important.
Living with Fibromyalgia
Living with fibromyalgia can be challenging, but strategies exist to help individuals cope with the condition and maintain a fulfilling life. Support groups and online communities provide a safe space for individuals to connect with others who understand their experiences, share coping strategies, and offer encouragement.
Educating oneself about fibromyalgia and its management is empowering. Knowing how to manage symptoms, communicate effectively with healthcare providers, and advocate for one’s needs can improve the overall quality of life.
Pacing oneself, setting realistic goals, and prioritizing self-care are crucial for managing the unpredictable nature of fibromyalgia. Building a strong support system, including family, friends, and healthcare professionals, can provide essential emotional and practical support. Is Fibromyalgia an Autoimmune Disease? ultimately affects how patients live with the condition.
Detailed Table Breakdown of Fibromyalgia Symptoms
| Symptom Category | Specific Symptoms |
|---|---|
| Pain | Widespread musculoskeletal pain, tenderness to touch, headaches |
| Fatigue | Persistent tiredness, lack of energy, difficulty concentrating |
| Sleep Disturbances | Insomnia, unrefreshing sleep, frequent awakenings |
| Cognitive Difficulties | Memory problems, difficulty concentrating, “fibro fog” |
| Mood Disorders | Anxiety, depression, irritability |
| Other Symptoms | Irritable bowel syndrome, restless legs syndrome, temporomandibular joint (TMJ) disorders |
FAQ: Frequently Asked Questions about Fibromyalgia and Autoimmunity
Is Fibromyalgia a Disability?
Whether fibromyalgia is considered a disability depends on the severity of symptoms and their impact on an individual’s ability to perform daily activities and work. Some individuals with severe fibromyalgia may qualify for disability benefits.
Can Fibromyalgia be Cured?
Currently, there is no cure for fibromyalgia. However, with appropriate management, symptoms can be significantly reduced, and quality of life can be improved.
Is Fibromyalgia Hereditary?
While fibromyalgia itself is not directly inherited, genetic factors can increase a person’s susceptibility to developing the condition.
Conclusion
So, is fibromyalgia an autoimmune disease? The answer remains complex and requires further research. While a definitive link hasn’t been established, evidence suggests a possible connection between fibromyalgia and immune system dysfunction. Understanding this connection is key to developing more effective treatments. Is Fibromyalgia an Autoimmune Disease? will remain a topic of discussion for some time. We hope this article has shed light on this important topic. We encourage you to explore other informative articles on our site to further expand your knowledge on health and wellness topics.
.
Is fibromyalgia an autoimmune disease? Get the facts on this chronic pain condition. Learn about symptoms, diagnosis, and the latest research.