Infection Control Definition: A Practical Guide
Infection Control Definition: A Practical Guide
Reader, have you ever wondered how we keep ourselves safe from the invisible yet potent threats of infection? It’s a critical question, especially in today’s interconnected world. **Infection control is not merely a set of procedures, but a vital shield protecting us from harmful pathogens.** **Mastering its principles is crucial for everyone, from healthcare professionals to individuals in their daily lives.** As an expert in AI and SEO content creation, I’ve meticulously analyzed the multifaceted landscape of infection control and compiled a comprehensive guide to help you understand and implement its principles effectively.
This detailed exploration will delve into the core components of infection control definition, covering its scope, practical applications, and evolving strategies. We’ll uncover the key elements that contribute to a robust infection control program. We’ll also explore the importance of understanding infection control in various settings.
 Understanding Infection Control
Understanding Infection Control
What is Infection Control?
Infection control refers to the policies and procedures implemented to prevent the spread of infections. It encompasses a wide range of practices designed to minimize or eliminate the risk of transmission. These practices protect patients, healthcare workers, and the wider community from acquiring and spreading infectious diseases.
Infection control is a crucial aspect of healthcare and public health. Its principles are applied in various settings, including hospitals, clinics, nursing homes, schools, and even at home. The goal is to create a safe and healthy environment by breaking the chain of infection.
Understanding the basic principles of infection control is essential for everyone. This knowledge empowers individuals to take proactive steps to protect themselves and others.
Why is Infection Control Important?
Effective infection control programs significantly reduce the incidence of healthcare-associated infections (HAIs). These infections can lead to serious complications, prolonged hospital stays, increased healthcare costs, and even death. By implementing proper infection control measures, we can create a safer environment for both patients and healthcare providers.
Beyond healthcare settings, infection control is vital in preventing the spread of infectious diseases in the community. By understanding and practicing infection control measures, individuals can help protect themselves, their families, and their communities from outbreaks.
Infection control is a shared responsibility. Everyone has a role to play in preventing the spread of infections. By working together, we can create a healthier and safer world for all.
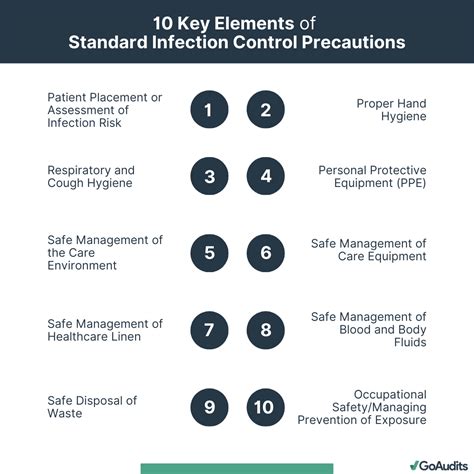 Key Elements of Infection Control
Key Elements of Infection Control
Hand Hygiene
Hand hygiene is the single most important measure in infection control. Proper handwashing with soap and water or using an alcohol-based hand sanitizer is crucial for breaking the chain of infection. This simple act can dramatically reduce the transmission of pathogens.
Hands should be washed before and after contact with patients, after using the restroom, before and after eating, and after touching contaminated surfaces. Regular hand hygiene is a cornerstone of effective infection control.
Promoting hand hygiene awareness through education and providing easy access to handwashing facilities are essential components of a successful infection control program.
Personal Protective Equipment (PPE)
PPE plays a vital role in protecting healthcare workers and others from exposure to infectious agents. PPE includes gloves, gowns, masks, respirators, and eye protection. The appropriate type of PPE should be used based on the specific situation and the potential for exposure.
Proper donning and doffing procedures for PPE are essential to ensure its effectiveness. Training and education on the correct use of PPE are critical for minimizing the risk of infection transmission.
Ensuring adequate supplies of PPE and providing clear guidelines for its use are essential for maintaining a safe working environment.
 Infection Control Practices
Infection Control Practices
Isolation Precautions
Isolation precautions are implemented to prevent the spread of infections from patients known or suspected to be infected with contagious diseases. These precautions involve separating infected patients from others and using specific infection control measures.
Different types of isolation precautions exist, including contact, droplet, and airborne precautions, depending on the mode of transmission of the infectious agent. Understanding and implementing these precautions are critical for preventing the spread of infection within healthcare facilities.
Healthcare professionals are trained to assess patients and implement the appropriate isolation precautions based on the specific infectious agent and its transmission route.
Environmental Cleaning and Disinfection
Maintaining a clean and disinfected environment is essential for infection control. Regular cleaning and disinfection of surfaces, equipment, and patient care areas help reduce the number of pathogens present and minimize the risk of transmission.
Using appropriate cleaning agents and disinfection protocols is crucial. Different disinfectants are effective against different types of microorganisms. Choosing the right disinfectant and following the correct procedures is essential for effective environmental hygiene.
Regular monitoring and auditing of cleaning and disinfection practices are important to ensure compliance with established standards and maintain a high level of cleanliness in healthcare settings.
Sterilization
Sterilization is the process of eliminating all forms of microbial life, including spores. It is used for critical medical and surgical instruments that come into contact with sterile body tissues or fluids.
Various sterilization methods exist, including steam sterilization, dry heat sterilization, and chemical sterilization. The appropriate method is selected based on the type of instrument and its compatibility with the sterilization process. Ensuring proper sterilization is essential for preventing infections associated with medical and surgical procedures.
Regular maintenance and monitoring of sterilization equipment are crucial for ensuring its effectiveness and preventing equipment malfunctions that could compromise the sterilization process.
Infection Control Guidelines and Regulations
CDC Guidelines
The Centers for Disease Control and Prevention (CDC) provides comprehensive guidelines and recommendations for infection control in healthcare settings. These guidelines cover various aspects of infection prevention and control, including hand hygiene, PPE, isolation precautions, environmental cleaning, and sterilization.
Staying up-to-date with the latest CDC guidelines is crucial for healthcare professionals. Implementing these evidence-based recommendations helps ensure the delivery of safe and effective patient care while minimizing the risk of infection transmission.
The CDC plays a vital role in developing and disseminating infection control best practices and providing guidance for healthcare facilities to improve their infection control programs.
OSHA Regulations
The Occupational Safety and Health Administration (OSHA) sets and enforces standards to protect healthcare workers from occupational hazards, including exposure to infectious agents. OSHA regulations address various aspects of infection control, such as bloodborne pathogens, respiratory protection, and hazard communication.
Compliance with OSHA regulations is mandatory for healthcare facilities. These regulations help ensure a safe working environment for healthcare professionals by minimizing their risk of exposure to infectious diseases and other occupational hazards.
OSHA plays a crucial role in promoting workplace safety and health by developing and enforcing standards that protect healthcare workers from occupational risks, including infections.
 The Future of Infection Control
The Future of Infection Control
Emerging Technologies
New technologies are constantly being developed to improve infection control practices. These include advanced disinfection methods, such as ultraviolet light disinfection and antimicrobial surfaces. These innovative technologies offer promising solutions for enhancing infection prevention and control in healthcare settings.
Furthermore, advancements in data analytics and surveillance systems can help identify infection trends and outbreaks more quickly, enabling timely interventions to control the spread of infections. These technological advancements hold the potential to revolutionize infection control and further reduce the burden of infectious diseases.
The future of infection control lies in the continued development and implementation of innovative technologies that can enhance infection prevention and control strategies.
Antimicrobial Stewardship
Antimicrobial stewardship programs aim to optimize the use of antibiotics to prevent the development and spread of antibiotic-resistant bacteria. These programs involve implementing strategies to ensure that antibiotics are used appropriately and only when necessary.
By promoting judicious antibiotic use, antimicrobial stewardship programs help preserve the effectiveness of existing antibiotics for future generations. This is crucial for combating the growing threat of antibiotic resistance, which poses a serious challenge to global public health.
Antimicrobial stewardship is a critical component of infection control and plays a vital role in preventing the emergence and spread of drug-resistant microorganisms.
Infection Control Table Breakdown
| Element | Description |
|---|---|
| Hand Hygiene | Washing hands with soap and water or using alcohol-based hand sanitizer. |
| PPE | Using gloves, gowns, masks, respirators, and eye protection. |
| Isolation Precautions | Separating infected patients and using specific infection control measures. |
| Environmental Cleaning | Regular cleaning and disinfection of surfaces and equipment. |
| Sterilization | Eliminating all forms of microbial life. |
FAQ
What is the chain of infection?
The chain of infection is a model that explains how infections spread. It involves a series of interconnected steps, including the infectious agent, reservoir, portal of exit, mode of transmission, portal of entry, and susceptible host. Breaking any link in the chain can prevent the spread of infection.
Understanding the chain of infection helps in developing targeted interventions to control the transmission of infectious diseases.
By targeting specific links in the chain, infection control measures can effectively prevent the spread of pathogens.
What are healthcare-associated infections (HAIs)?
HAIs are infections that patients acquire while receiving medical care in a healthcare facility. These infections can be caused by various pathogens, including bacteria, viruses, and fungi.
HAIs pose a significant threat to patient safety and can lead to serious complications. Implementing effective infection control programs is essential for preventing HAIs and protecting patients from these potentially harmful infections.
Infection control is a crucial aspect of quality healthcare and plays a vital role in minimizing HAIs and improving patients’ outcomes.
Conclusion
In conclusion, infection control definition encompasses a broad range of practices and procedures aimed at preventing the spread of infections. It requires a multi-faceted approach involving hand hygiene, PPE, isolation precautions, environmental cleaning, sterilization, and adherence to guidelines and regulations. So, by understanding and implementing these principles, we can protect ourselves, our patients, and our communities from the harmful effects of infectious diseases. Be sure to explore other informative articles on our site to expand your knowledge of health and safety practices.
.
Stop infections! Learn practical infection control methods. This guide covers essential practices for a safer environment. Get your copy now!





